Glioblastoma is an aggressive brain cancer with a median survival of just 15 months. Multi-pronged efforts are underway to improve the effectiveness of post-surgical radiation treatment, such as dose escalation, where increased dose is delivered to regions of treatment-resistant tumour. However, this approach requires the ability to rapidly and easily identify tumours that are not responding to radiotherapy.
With this aim, researchers at the University of Toronto’s Sunnybrook Health Sciences Centre have investigated whether diffusion-weighted imaging (DWI) on an MRI-guided linear accelerator (the 1.5 T Unity MR-Linac) can be used to identify such dose escalation targets.
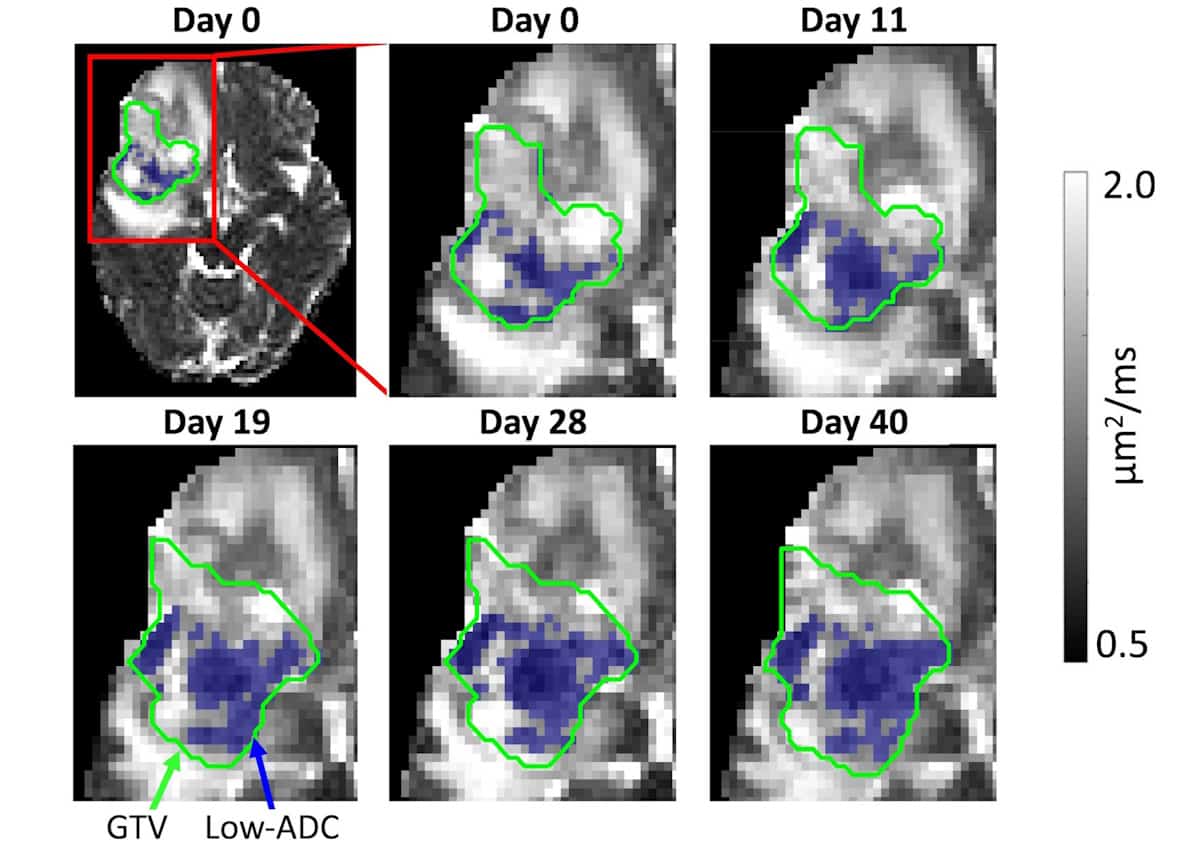
DWI generates MR contrast based on the diffusion of water molecules, with in vivo diffusivity quantified via a parameter called the apparent diffusion coefficient (ADC). Cell membranes restrict water diffusion, resulting in low ADC values. Thus tumour regions of low ADC may indicate highly cellular, dense tumour. A reduction in low-ADC regions during radiotherapy could imply a decrease in solid tumour, while increasing low-ADC volume could indicate that a tumour is not responding to treatment.
First author Liam Lawrence and colleagues investigated whether changes in ADC, identified via daily MR-Linac DWI during treatment, were prognostic for survival. They found that changes in low-ADC regions correlated more strongly with survival than changes in the gross tumour volume (GTV), reporting their findings in Radiotherapy and Oncology.
The study included 75 patients diagnosed with glioblastoma who underwent chemoradiotherapy, 32 of whom were treated on the Unity MR-Linac and 43 with a conventional linear accelerator. All patients were imaged with simulation MRI scanners (MR-sim) at treatment planning, and at weeks 2, 4 and 10 after treatment started.
The researchers analysed 479 DWI scans from the MR-Linac and 289 DWI datasets from MR-sim scans, using voxel-wise fitting to generate ADC maps. They defined “low-ADC” tumour regions as voxels within the GTV with ADC of less than 1.25 µm2/ms. This threshold identifies dense and non-necrotic tumour and is greater than the mean ADC of high-grade glioma.
For both the low-ADC region and the GTV, the researchers computed the median volume changes at each timepoint over all patients. They then classified each patient as exhibiting a volume change above or below this median. They also divided patients into “good” and “poor” response groups, based on whether overall survival and progression-free survival were more or less than 14.6 and 6.9 months, respectively.
Both MR-Linac and MR-sim measurements showed that the low-ADC region decreased in volume as treatment progressed. In the MR-Linac DWI cohort, low-ADC volume changes differed significantly between patients exhibiting early and late tumour progression (at weeks 1, 2, 3 and 5 for the MR-Linac DWI data, and weeks 2, 4 and 10 for MR-sim data). Using the MR-sim data from all patients, the low-ADC changes differed between good and poor responders at weeks 2, 4 and 10.

Is the MR-linac the future of adaptive radiotherapy?
The researchers report that low-ADC volume changes two to five weeks from the start of radiotherapy showed an association with overall survival for the MR-Linac DWI cohort, although they did not identify any correlation with progression-free survival. They note that MR-sim-based low-ADC changes showed greater correlation with overall and progression-free survival than GTV changes.
“Regions of low diffusivity identified with DWI are potential candidates for dose escalation, as they may represent solid, residual tumour,” the authors write. “Furthermore, regions of low ADC that remain after several weeks of radiation may reflect tumour that is resistant to treatment. Changes in low-ADC regions correlated more strongly with survival than changes in the contrast-enhancing GVT and clinical factors. The results of the present study and previous ones imply that DWI might allow mid-treatment response assessment, which would enable early salvage therapy if first line therapy is ineffective.”
- SEO Powered Content & PR Distribution. Get Amplified Today.
- PlatoData.Network Vertical Generative Ai. Empower Yourself. Access Here.
- PlatoAiStream. Web3 Intelligence. Knowledge Amplified. Access Here.
- PlatoESG. Carbon, CleanTech, Energy, Environment, Solar, Waste Management. Access Here.
- PlatoHealth. Biotech and Clinical Trials Intelligence. Access Here.
- Source: https://physicsworld.com/a/imaging-on-an-mr-linac-identifies-radiation-resistant-brain-tumours/
- :is
- :not
- :where
- 1
- 10
- 14
- 15%
- 2023
- 23
- 25
- 32
- 75
- 9
- a
- ability
- above
- accelerator
- adaptive
- After
- aggressive
- aim
- All
- allow
- also
- Although
- an
- and
- any
- apparent
- approach
- ARE
- AS
- assessment
- Association
- At
- author
- authors
- based
- BE
- below
- between
- Blue
- both
- Brain
- brain cancer
- CA
- called
- CAN
- Cancer
- candidates
- change
- Changes
- classified
- click
- Clinical
- Cohort
- colleagues
- contrast
- conventional
- Correlation
- could
- daily
- data
- datasets
- decrease
- decreased
- defined
- delivered
- DID
- Diffusion
- divided
- dose
- during
- each
- Early
- easily
- effectiveness
- efforts
- enable
- escalation
- Exhibiting
- factors
- findings
- First
- fitting
- five
- For
- found
- from
- future
- generate
- generates
- good
- greater
- gross
- Group’s
- Growth
- Have
- Health
- highly
- However
- HTTPS
- identified
- identifies
- identify
- if
- image
- Imaging
- improve
- in
- included
- increased
- increasing
- indicate
- information
- into
- issue
- jpg
- just
- Late
- less
- Line
- Low
- Maps
- max-width
- May..
- mean
- measurements
- might
- months
- more
- mr
- MRI
- of
- on
- ones
- open
- or
- over
- overall
- parameter
- patient
- patients
- Physics
- Physics World
- planning
- plato
- Plato Data Intelligence
- PlatoData
- poor
- potential
- present
- previous
- progressed
- progression
- Radiotherapy
- rapidly
- recorded
- reduction
- reflect
- region
- regions
- remain
- report
- Reporting
- represent
- requires
- researchers
- resistant
- respectively
- responding
- response
- restrict
- resulting
- Results
- SCIENCES
- seen
- several
- showed
- shown
- significantly
- simulation
- solid
- start
- started
- strongly
- Study
- such
- survival
- targets
- than
- that
- The
- The Future
- their
- then
- they
- this
- threshold
- thumbnail
- Thus
- to
- treatment
- true
- two
- Underway
- underwent
- unity
- used
- using
- Values
- via
- volume
- Voxels
- Water
- Weeks
- were
- whether
- which
- while
- WHO
- with
- within
- world
- would
- write
- zephyrnet